By Leanna Coy, FNP-BC
Under the Affordable Care Act (ACA) and the expansion of Medicaid, 44 million people gained health insurance. This allowed people who were unable to get medical coverage through their work, those with pre-existing conditions, and young adults to access affordable healthcare. But that is all about to change with the passing of the “One Big Beautiful Bill.”
The reconciliation law, also known as the One Big Beautiful Bill (OBBB), was signed on July 4, 2025. Touted as a method of creating economic growth for the United States, the bill will end up costly for Americans. Under the bill, one major area of change is the $863 billion in cuts to Medicaid. President Donald Trump has said he “loves Medicare and Medicaid,” but pushed for the passage of this bill that will result in millions of Americans losing their health coverage. In rural areas, like Tillamook County, people will get hit the hardest.
Oregon’s Medicaid Program
Medicaid is a program that helps cover medical expenses for individuals who have limited income and resources. Different states have different names for their Medicaid programs. In Oregon, it is known as the Oregon Health Plan (OHP). OHP currently covers 1.4 million Oregonians. In Tillamook County, 35.8% of the population is enrolled in OHP. OHP covered services include mental health care, treatment for substance use disorder, prenatal care, prescriptions, preventative care, emergency care, and more.
Oregon is one of the most vulnerable states for people to lose their Medicaid coverage due to Oregon’s expansion of Medicaid. The state made it easier for people to enroll and stay enrolled in OHP, resulting in more individuals having access to medical coverage. The OBBB cuts to Medicaid will reduce or eliminate much of the funding that is currently covering Oregonians who received coverage under the expansion.
Pending Cuts to Medicaid
Both the federal and state governments fund Medicaid. The federal government pays a federal match rate, known as FMAP, to the forty-one states that have implemented the Affordable Care Act’s Medicaid expansion. The FMAP currently pays 90% of the cost for people who enrolled in the Medicaid expansion. Approximately one-quarter of people using Medicaid are covered under the expansion.
The OBBB includes what are being called catastrophic cuts to Medicaid at the federal level. The Congressional Budget Office (CBO) estimates the cuts will leave an additional 10 million people without health insurance by 2034. Add to this the expiring tax credits for health insurance from the ACA set to expire at the end of this year, and that number rises to more than 14 million. The cuts are scheduled to begin in 2026 and are spread out over 10 years. An estimated 20% of Oregon’s population will be affected by cuts to Medicare.
The Impact on Rural Oregon
When the cuts to Medicaid take effect, rural areas will be hit particularly hard. Rural communities have higher percentages of people utilizing OHP at 31.1% compared to 25.5% in urban areas. Loss of funding is not the only factor. The OBBB sets new restrictions for someone to qualify for Medicaid. These restrictions don’t simply make it harder for someone to become eligible for OHP, but also more difficult for them to stay eligible.
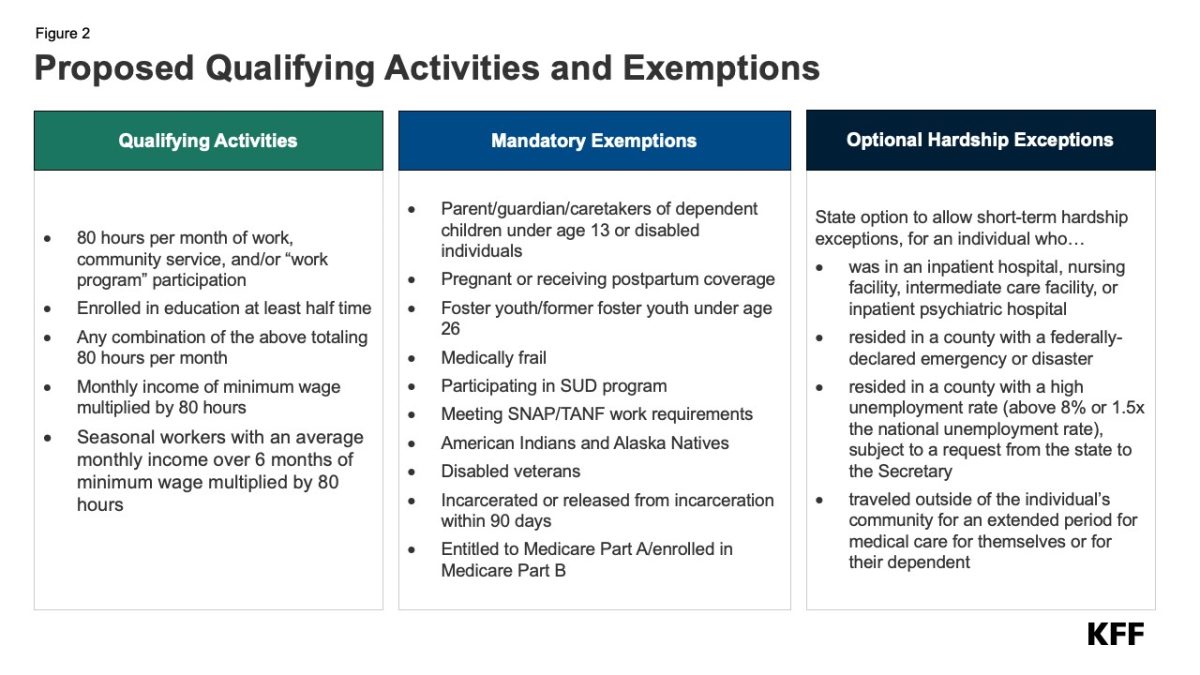 To qualify, adults ages 19 to 64 will be required to complete 80 hours of work, volunteer service, or school each month. This will be hard for many people to track if they don’t clock in or out for work or have a human resources department managing the paperwork. Additionally, instead of renewing once a year to maintain OHP, individuals will be required to requalify every 6 months. These changes put the seasonal workers, timber families, and fishing families in the off-season, and those who rely on tourism dollars are at most risk in Tillamook County. For those who work less than full-time, their benefits will be cut.
To qualify, adults ages 19 to 64 will be required to complete 80 hours of work, volunteer service, or school each month. This will be hard for many people to track if they don’t clock in or out for work or have a human resources department managing the paperwork. Additionally, instead of renewing once a year to maintain OHP, individuals will be required to requalify every 6 months. These changes put the seasonal workers, timber families, and fishing families in the off-season, and those who rely on tourism dollars are at most risk in Tillamook County. For those who work less than full-time, their benefits will be cut.
A Flawed Plan
Work requirements for Medicaid coverage have been attempted at the state level, but they always fail. At this time, Georgia is the only state with a work requirement for Medicaid coverage, and their enrollment is falling considerably short of its need. Currently, only 8,000 people have health care coverage under Medicaid out of the 240,000 who need it in Georgia. When the state implemented work requirements, the number of covered people dropped dramatically. More than 40% of the counties had fewer than 10 enrollees after the first year because of difficulties with the work requirements. Yet, for only 8,000 enrollees, the state has spent $110 million.
Georgia’s program presents numerous obstacles for its citizens to maintain Medicaid coverage. These include computer glitches, a lack of customer service, difficulty for users to load the necessary documents to meet the requirements, and an absence of high-speed internet in many areas.
Users who rely on volunteer hours to qualify have also experienced problems. In rural areas, volunteer opportunities are often limited. The increased demand for volunteer hours has created a strain for organizations to track and submit these hours to the state. Making tracking more burdensome is that the state has failed to develop a standard form for volunteer organizations to use to track hours. This means it is easier for the necessary information to be missed and for Medicare to be denied. The state has enrollment navigators to assist with these issues, but a shortage of staff already exists, and federal funding cuts in 2026 will worsen the shortage.
Pressure on An Already Suffering Healthcare System
The changes to Medicaid will also have broader implications for local health care, as less money will go into the health care system. Currently, Medicaid dollars account for $1 out of every $5 spent on healthcare. This means that clinics and hospitals, which are already struggling, will experience even more difficulties. We may see more closures and less access to services. The recently announced closure of the labor and delivery unit at Providence Seaside may be an omen. Often, labor and delivery are just the first services cut when hospitals begin to lose dollars.
A loss of services often has a domino effect, leading to more trouble recruiting and maintaining medical staff. Something Providence has cited as a reason for the department closure. “We have struggled to recruit providers and staff, and our only OB/GYN physician retired Aug. 1, 2025. Despite our efforts, we have been unsuccessful in recruiting a new OB/GYN for nearly two years.”
Local clinics that will feel the most impact are the Federally Qualified Health Centers (FQHCs). These include the Tillamook County Community Health Centers and the Nehalem Bay Health Center and Pharmacy. FQHCs are health centers that receive federal dollars to provide health care to underserved areas for anyone who needs it. The care can include primary care, behavioral health, maternal care, and dental treatments.
The cuts to Medicaid will reduce the funds these clinics receive. Less funding may impact services due to the limited availability of funds for staff salaries and resources. The OBBB cuts also include reducing loan repayment for healthcare providers, which has historically been a draw for providers to work in FQHCs. These two factors may lead to fewer healthcare providers and staff to keep the clinics open.
Oregon has a long history of working to provide medical coverage for its citizens. The OBBB delivers a massive blow to these efforts and will lead to worse health outcomes for millions of people. Far from reducing costs, the OBBB is estimated to increase deficits by $3.4 trillion over the next 10 years. These are costs Oregonians cannot afford to endure.

.png)