By Leanna Coy, FNP-BC
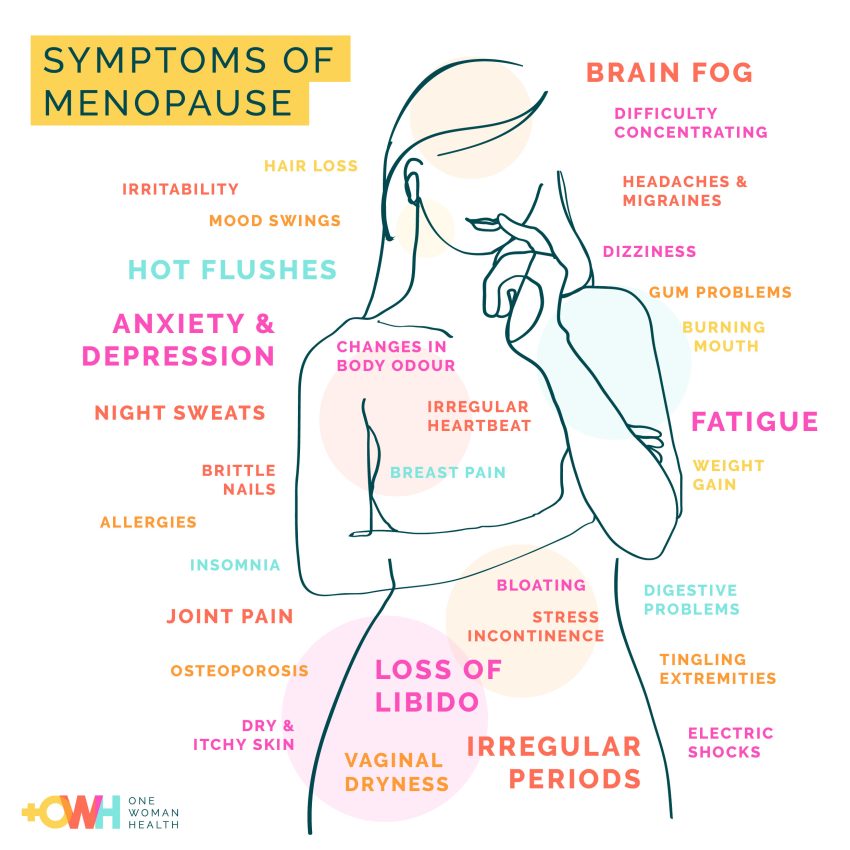
Women (people born with ovaries) experience many physical changes when their estrogen begins to decline in perimenopause. Some are obvious, such as hot flashes and weight gain in the belly. Others are a bit more insidious and may go unrecognized for years. One such area is the vulva. The vulva goes through changes that range from mild irritation to outright pain and changes to the physical architecture. Yes, menopause is again bearing gifts. Let’s dive into this sensitive, but essential topic.
What is the vulva?
The vulva is the formal term for the external female genitalia found between your legs. There is more to this area than the vagina. The vulva also has the:
- Urethral opening: where urine (pee) exits the body
- Labia minor and majora: plump skin folds that cover and protect the inner parts
- Vaginal opening: where menstrual blood passes out of the body, and where a baby is delivered through
- Clitoris: the pleasure center for the body
- Mons pubis: the mound of hair covered fatty tissue covering the pubic bone
- Perineum: the space between the vaginal opening and the anus
How the vulva changes
We all know estrogen as the female hormone. When we are young, estrogen helps to develop our sexual characteristics, such as breast development. With the vulva specifically, estrogen causes the parts to mature and hair to grow.
In adult women, the role of estrogen in the vulva is to maintain blood flow, moisture, and the thickness of the tissues. As the estrogen levels begin dropping and become less consistent in perimenopause, changes begin. The skin of the vulva starts to thin and become less elastic. Dryness and lack of vaginal lubrication occur. There is a loss of fat padding, and the tissues become more easily irritated. There is some loss of sensation leading to decreased ability to become aroused and/or enjoy sex. The actual architecture of the vulva changes in what used to be called “vaginal atrophy.” These changes are known as genitourinary symptoms of menopause (GSM).
More than half of all women will develop GSM. For most women, these changes begin in their 40s. However, some will start experiencing changes in their late 30s. Vaginal dryness is often the first sign. The shifts that occur with these changes can be dramatic and quite noticeable, or subtle changes that may go unnoticed for years. Common symptoms include:
- Vulvar itching
- Persistent burning or irritation
- Vaginal dryness
- Pain or discomfort with sex
- Change in odor
- Discomfort with sitting for long periods
- Increased frequency of urinary tract infections (UTIs)
How to get relief
Due to the declining estrogen levels in the body, these changes are progressive. This means they will continue to worsen with aging. Treating the symptoms will provide some relief, but treatment needs to continue indefinitely.
How to care for yourself
- Self-care starts with the use of vaginal moisturizers. These are not lubricants. Lubricant is for sex. Moisturizers are for self-care. They help retain moisture in the vulva and vaginal area to reduce discomfort and dryness. These are available at the pharmacy.
- Gentle soaps.
- If no one has ever told you this before, avoid douching. ALWAYS. Douching washes away both bad and good bacteria. Your vagina is a self-cleaning oven. You don’t need to douche. Ever.
- Stay sexually active. Sexual activity promotes blood flow and helps maintain the elasticity of the tissue, which helps reduce dryness, irritation, and pain. For those without a partner, masturbation counts in promoting these benefits. Research found that women with regular sexual activity had fewer GSM symptoms.
- Wear breathable clothing, such as cotton underwear.
How your healthcare provider can help
The good news is that treatments are available. Talk with your healthcare provider at the first signs of GSM symptoms. This can be your gynecologist or primary care provider. Some women find it hard to talk about issues they see as “private.” But having an open conversation will help the healthcare provider understand what you are experiencing and address your concerns adequately. They can also help rule out other potential causes, such as vaginal infections. Your healthcare provider can work with you on finding a treatment that aligns with your health and physical needs. Some treatments include:
- Systemic hormone therapy started early in perimenopause. Treatments include estrogen patches, pills, and gels.
- Vaginal estrogens to help target the problem area. These tend to be local and are safe to use in addition to systemic therapy. These include topical creams, vaginal suppositories, and vaginal rings.
Unfortunately, I hear from women all the time that their provider just dismisses their concerns. If you don’t feel comfortable or heard by your provider, consider speaking with a menopause specialist.
The vulvar changes women experience in menopause are an unfortunate, but normal part of the changes. No one needs to feel like they must suffer with the symptoms. You only have one body to take care of, and these changes aren’t going to get better with the passage of time. Talk with your provider and get started on your vulvar self-care.
Series of articles about Menopause & Perimenopause:
– https://www.tillamookcountypioneer.net/in-good-health-not-just-hot-flashes-what-every-woman-should-know-about-the-perimenopause-transition/
– https://www.tillamookcountypioneer.net/in-good-health-perimenopause-impacts-the-word-is-on-the-tip-of-my-tongue-brain-fog/